By Dr. Richard Thompson, DC
3 Minute Read

When this type of clinical picture presents during a consultation, I immediately start to question the patient as to what has changed in their daily activity and exercise regimens. When injuries occur gradually, compared to an acute onset that brings pain immediately such as a sprained ankle, we have to try to identify what factors would have led to dysfunction in the body. Injury doesn’t occur without a reason behind it. When pain builds gradually, it usually means that something has led to the body not being able to accommodate that change from a functional movement perspective. The possibilities of such changes are endless – changes in footwear, training intensity, training volumes, training terrain (road vs. trail running), the body’s hydration, and changes in activities of daily living, such as an increase in sitting throughout the day. Any and all of these factors can lead to new stress on how the body moves, which can eventually lead to dysfunction in the tissues, such as the muscles, fascia (connective tissue), and joint capsule. Once dysfunction develops and goes unaddressed over a period of time, the body is at increased risk of developing pain and injury.
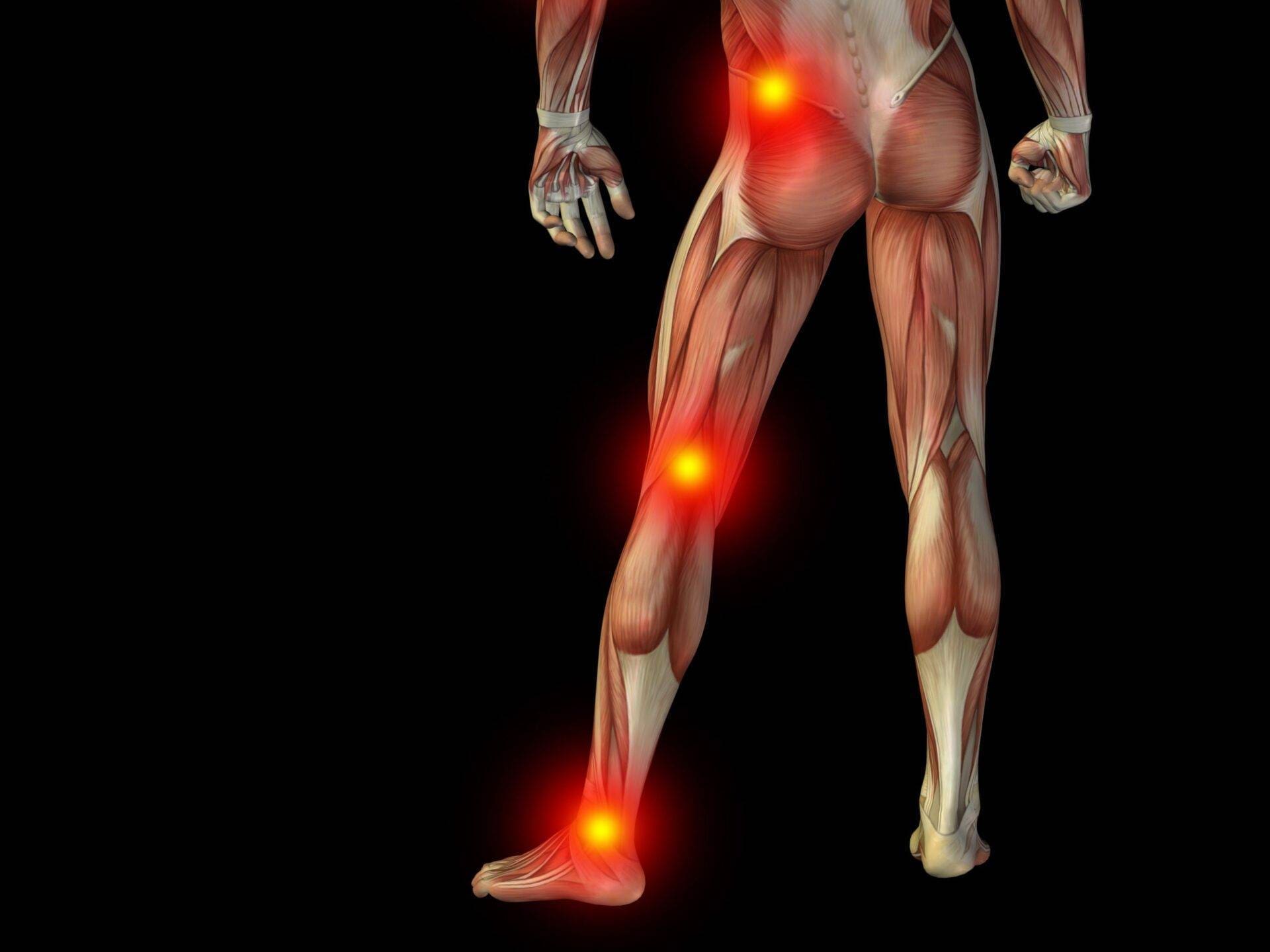
You may be asking WHY the problem at the hip leads to knee pain. I like to describe this situation as the knee being the innocent bystander and the hip being the true culprit. Biomechanically, the knee joint is a hinge joint that mostly flexes (bends) and extends (straightens). It is located between two much more complex joints – the ankle and the hip. With weight-bearing exercise, where the weight of the body is loaded on the entire lower limb, the ankle-knee-hip complex is considered a closed-chain system. This means what happens at the ankle joint has an impact all the way up the leg, as far up as the low to mid-back, and vice versa. So how does this cause the hip to affect the knee? When dysfunction builds in the structures around the hip, such as the hip rotator muscles, this causes a change in the femur’s (upper leg) movement pattern either due to a restriction in movement from tissue contracture or excessive movement from inhibited (weakened) muscle activity. This change in femur movement now causes the innocent knee joint to start to move abnormally, with increased rotational stress at the knee, leading to pain due to aberrant movement. This is often referred to as patellofemoral joint syndrome. In this case, the solution is to address the dysfunction at the hip, and the symptoms at the knee will correct themselves.

Patients are commonly very frustrated with this type of injury as they are often trying to address the problem at the knee, where the true issues lie higher up at the hip. If you think you are experiencing this type of problem, introduce regular stretching for the hip and buttocks. If that does seem to address your knee pain, seek help from a healthcare provider to assess and diagnose the problem. Although this may seem to be a complex issue, addressing the source of the problem often helps resolve the issue effectively and quickly.

